As the seasons change and temperatures rise, many folks wonder: does blood thin in warm weather? While it may seem like a simple question, delving into the intricacies of human physiology unveils a fascinating tapestry of responses that our bodies exhibit in reaction to heat. To appreciate this phenomenon, one must explore the composition of blood, the ways in which our body regulates temperature, and the potential implications of these changes on our overall health.
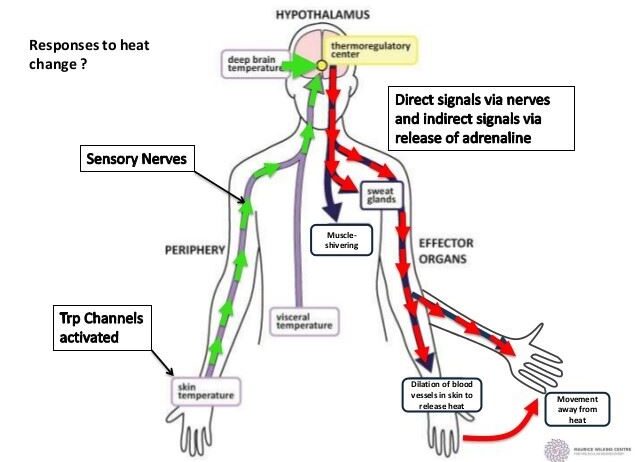
The human body is a remarkable system that maintains a stable internal environment—a process known as homeostasis. When ambient temperatures soar, the mechanisms employed to keep our core temperature regulated initiate a complex series of biological adaptations.
First and foremost, blood serves as an essential transport medium. Comprising red blood cells, plasma, white blood cells, and platelets, blood fulfills various vital roles, including oxygen transport, nutrient delivery, and waste removal. The intriguing interplay between heat and blood viscosity—the thickness or thinness of blood—begins here.
In warm weather, the viscosity of blood is influenced by a multitude of factors. One major component is plasma volume. Warm temperatures lead to sweating, which is the body’s primary means of thermoregulation. When the body loses water through perspiration, plasma volume decreases, potentially increasing the concentration of red blood cells. This concentration elevates blood viscosity temporarily, a phenomenon that may counterintuitively appear to contradict the notion of “thinning.” However, it’s essential to recognize the adaptive capacity of the body to mitigate such changes.
As temperatures continue to rise, the body experiences vasodilation, the process of widening blood vessels. Vasodilation enhances blood flow to the surface of the skin, facilitating heat dissipation. The increased blood flow acts to lower core temperature by allowing thermal energy to escape through the skin. Interestingly, during this process, the blood exhibits a lower resistance to flow due to the increased width of blood vessels, which can feel like a “thinning” effect. Thus, while the viscosity of blood may increase initially due to dehydration, the subsequent physiological responses create a paradox: enhanced blood flow in warmer conditions can lead to somewhat reduced resistance, making it feel thinner as it circulates more freely.
But does this mean that maintaining hydration in the heat is dispensable? Not at all. In fact, the challenges of heat stress necessitate an increased focus on hydration to assist the body’s ability to regulate temperature effectively. When dehydrated, the body is at risk for diminished performance, increased fatigue, and potentially serious conditions such as heat exhaustion or heat stroke. As blood becomes thicker due to reduced plasma volume, the heart must work harder to pump this thicker substance through the circulatory system. This increase in workload can be taxing, particularly for those with pre-existing cardiovascular conditions, and thus eating well and hydrating properly becomes crucial during the sweltering days of summer.
Additionally, there is an interesting consideration regarding how blood composition can change based on heat exposure. The body actively adjusts red blood cell production in response to temperature changes, particularly at notable altitudes or during prolonged exposure to heat. An acclimatized individual may experience a higher propensity for red blood cell synthesis, which in turn can optimize oxygen delivery during physical activities in warmer conditions. This adaptation suggests that the body is not a static entity; it continuously evolves in response to its environment, demonstrating resilience and versatility.
However, challenges do arise. In individuals with certain medical conditions, such as sickle cell disease, changes in blood viscosity can pose significant risks. The warmer weather may exacerbate symptoms, leading to vaso-occlusive crises due to the interaction of heat, dehydration, and blood flow dynamics. Such cases highlight the importance of individualized medical considerations in situations of heat stress.
Encouragingly, modern advancements in sports science and medicine are tapping into our understanding of human physiology during heat exposure. For athletes, maintaining volume through preemptive hydration strategies has become a cornerstone of performance optimization. Creatively prescribed hydration protocols, often emphasizing electrolyte balance, can mitigate the adverse effects of heat, ensuring that blood remains adequately voluminous and less viscous despite the rising temperatures.
With the ongoing discussions surrounding climate change and fluctuating weather patterns, an often overlooked but critical dialogue centers around the relationship between heat and human physiology. We must consider the broader implications of increasing global temperatures. How might variations in heat exposure impact public health on a larger scale? Will more individuals face challenges related to blood viscosity and circulatory health? These questions beckon exploration and proactive measures to ensure that individuals thrive amid changing climates.
In conclusion, while the inquiry into whether blood thins in warm weather may lead to nuanced discussions of viscosity, thermoregulation, and hydration, it unequivocally nudges us to reassess our resilience and responses to heat. As we navigate through the hotter seasons ahead, the interplay of heat and human physiology remains a compelling area of study, essential for maximizing health and performance during the sweltering months. For every rise in temperature, we invite a deeper understanding of our biological adaptability, and foster a call to action for increased awareness among the public about the significance of maintaining hydration and healthy blood flow as crucial components of our well-being.