As summer approaches and temperatures soar, many individuals find themselves pondering the implications of heat on their bodies. One perennial question arises: does your blood thin in hot weather? This inquiry not only prompts scientific curiosity but also invites consideration of how our physiological responses adapt to climatic variations. Exploring this topic unveils a complex interplay between temperature, blood viscosity, and overall health during those sweltering months.
To grasp the intricacies of how heat affects the human body, one must first understand the fundamental properties of blood. Blood is a viscous fluid comprised primarily of plasma, red blood cells, white blood cells, and platelets. The viscosity of blood is influenced by various factors, including hydration levels, temperature, and the concentration of blood components. When one asks if blood thins in hot weather, it’s crucial to clarify what is understood by “thinning.” In a physiological context, thinning implies a reduction in blood viscosity.
When exposed to high temperatures, the body engages in several adaptive mechanisms. Primarily, it works to regulate its internal temperature through the process of sweating. As sweat evaporates from the skin’s surface, it removes heat from the body, thus cooling it down. This physiological response also leads to increased fluid loss; dehydration can occur swiftly if adequate hydration is not maintained. When individuals drink water or electrolyte solutions to replenish lost fluids, the blood volume increases. In a sense, this can lead to a temporary decrease in blood viscosity. However, this phenomenon is not a direct result of the heat “thinning” the blood but rather the result of proper hydration management.
Contradicting the oversimplified notion of thinned blood is the complex reality of blood viscosity. High temperatures can initially decrease blood viscosity due to increased hydration from fluid intake. However, the effect of extreme heat on blood viscosity is nuanced. Prolonged exposure to high temperatures can lead to dehydration, resulting in a thickening of the blood. When fluid levels dwindle, blood can become more concentrated, thereby increasing viscosity. This paradox highlights the critical need for individuals to remain hydrated in scorching conditions.
Let us delve deeper into the implications of these changes. Increased blood viscosity due to dehydration can pose significant health risks. It may lead to elevated blood pressure and strain on the cardiovascular system. The consequences are especially pronounced for individuals with pre-existing conditions, such as hypertension or cardiovascular disease. The heart must work harder to pump thicker blood, which can exacerbate these health issues. Thus, while it’s tempting to consider blood thinning as a straightforward advantage of rising temperatures, the actual health landscape is far more complex.
Moreover, the effects of summer heat aren’t just limited to blood viscosity. Heatwaves can trigger various physiological responses, including increased heart rates and altered metabolic functions. Consequently, the cardiovascular system must navigate through these challenges judiciously. The heart works harder during hot weather to maintain an adequate supply of oxygen and nutrients, which intensifies the risk of heat-related illnesses, such as heat exhaustion or heat stroke. As such, it becomes evident that simplistic answers about blood thinning overlook essential details regarding how the body copes under duress.
Research has shown that ambient temperatures also impact the body’s thermoregulatory mechanisms. When external temperatures rise, the body’s ability to resolve thermal loads is critical. Blood vessels dilate in a process known as vasodilation, allowing more blood to flow nearer the surface of the skin to enhance heat loss through radiation and convection. This phenomenon is particularly vital for maintaining thermal equilibrium. However, in severe heat conditions where shade and hydration might be limited, the risk of overheating becomes a pressing concern. Thus, with the cardiovascular system under strain, ensuring proper hydration becomes an imperative strategy.
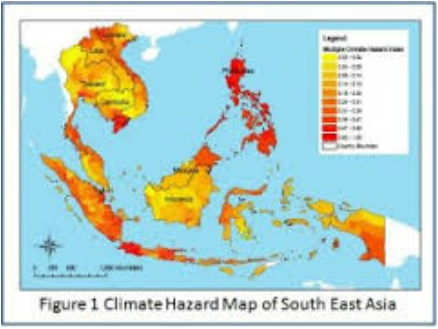
Importantly, individuals’ responses to heat are not uniform. Factors such as age, fitness level, and acclimatization play significant roles in how the body manages heat stress. Young, healthy individuals may effectively toggle between vasodilation and increased sweating, while older adults or those with chronic health conditions may struggle to modulate their body temperature effectively. Such disparities emphasize the need for a tailored approach to health during hot weather, particularly for vulnerable populations.
In conclusion, the question of whether blood thins in hot weather invites closer examination of the interdependent processes at play within the human body. While mild heat exposure in combination with proper hydration may temporarily reduce blood viscosity, excessive heat without adequate fluid intake leads to dehydration and increased blood viscosity. The nuances of these physiological responses underscore the critical importance of adapting to seasonal changes while maintaining a vigilant approach to hydration and overall health. Rather than oversimplifying with the notion that heat permanently thins the blood, one should embrace a more holistic understanding of how our bodies adapt to the demands placed upon them by extreme temperatures.
As we anticipate the summer sun and its heat, it’s imperative to remain proactive about hydration and be aware of the signs of heat-related illnesses. Ultimately, such knowledge equips us to navigate the challenges posed by summer temperatures while preserving our health and well-being.