The phenomenon of heatwaves has garnered increasing attention in recent years, not merely as a transient climatic event but as a harbinger of the alarming realities of global warming. The intricacies of this matter unfurl a tapestry of concern, especially regarding its insidious repercussions on public health and the healthcare infrastructure. This intersection of extreme weather and healthcare poses a multifaceted challenge that necessitates urgent discourse and intervention.
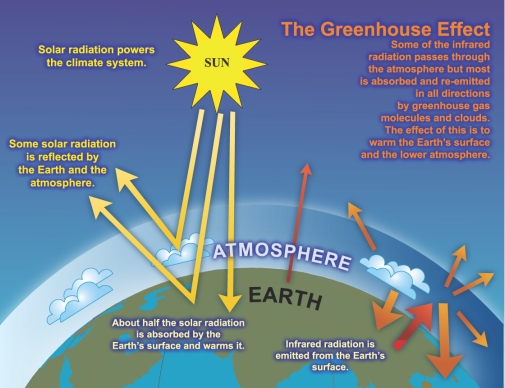
Heatwaves, characterized by prolonged durations of excessively high temperatures, have become more frequent and severe, directly correlating with anthropogenic climate change. The escalating incidence of such extreme weather events can be attributed to several factors, including greenhouse gas emissions, urbanization, and deforestation. Consequently, the increased thermal stress exposed to populations is not just a discomfort but a potential catalyst for a plethora of health issues.
In urban environments, the so-called “urban heat island” effect exacerbates the situation. Cities, with their concrete and asphalt, tend to absorb and retain heat, leading to higher temperatures relative to their rural surroundings. This phenomenon can significantly impact vulnerable demographics, such as the elderly and those with pre-existing health conditions, creating an urgent need for adequate healthcare response systems.
The immediate health implications of heatwaves are manifold. Elevated temperatures can precipitate heat-related illnesses, including heat exhaustion and heat stroke. Such conditions demand prompt medical intervention. Hospitals, already under strain due to growing patient loads, could quickly become overwhelmed during extreme heat events. Emergency departments may face a deluge of patients presenting with heat-related complications, thereby diverting resources from other critical healthcare needs.
Beyond acute illnesses, the long-term health consequences of heatwaves warrant serious consideration. Research indicates a correlation between prolonged exposure to high temperatures and chronic health issues, such as cardiovascular and respiratory diseases. Vulnerable populations, already facing barriers to accessing care and preventive services, are disproportionately affected. This exacerbation of health disparities highlights systemic failures in healthcare delivery that must be addressed in tandem with climate action.
Moreover, the interplay between heatwaves and mental health is an often-overlooked dimension of this crisis. Extreme heat can exacerbate conditions like anxiety and depression, leading to increased rates of hospitalizations for mental health emergencies. The stress of surviving oppressive heat can contribute to higher instances of substance abuse, sleep disorders, and general malaise, creating a cyclical burden on healthcare systems already stretched thin.
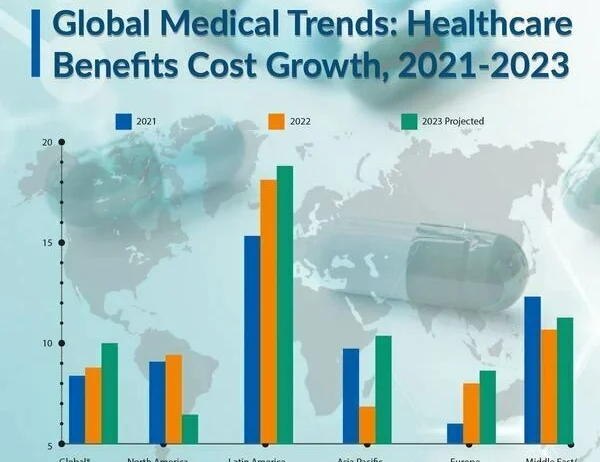
As the ramifications of heatwaves become increasingly dire, hospital infrastructure itself may experience palpable strain. Rising temperatures necessitate more efficient cooling systems in healthcare settings. Facilities may need to recalibrate their operational protocols to accommodate surges in patient numbers during heat events. However, these measures often come with significant financial implications, exacerbating the already high costs associated with healthcare delivery.
The financial burden placed on healthcare systems due to heatwaves is another critical aspect to consider. The economic ramifications of increasing heat-related healthcare costs manifest in a multitude of ways. As patient admissions surge during heatwaves, operational costs rise, potentially leading to higher insurance premiums and out-of-pocket expenses for patients. This can deter individuals from seeking necessary care, creating a dangerous paradox where financial considerations exacerbate health outcomes.
Policy initiatives aimed at mitigating the impact of heatwaves on health are imperative and must be multidimensional. First, there is an urgent need for a comprehensive public health response, including heat-health action plans that incorporate community engagement. Health departments must pivot to develop strategies aimed at identifying vulnerable populations and ensuring they have access to cooling resources, medical care, and information regarding heat safety.
Additionally, integrating climate resiliency into healthcare planning can yield profound benefits. Hospitals and clinics should be designed or renovated to withstand extreme heat scenarios, prioritizing sustainable building materials and energy-efficient cooling technologies. Furthermore, urban planning must incorporate green spaces, reflective materials, and other heat-mitigating strategies to reduce the urban heat island effect and promote overall community health.
Collaboration between various sectors is crucial in creating an effective response to the health crises stemming from heatwaves. Stakeholders, including public health officials, urban planners, and environmental advocates must align their initiatives. Educational campaigns aimed at raising awareness about the dangers of heatwaves and instilling heat safety practices can empower communities to take proactive measures against the heat.
Finally, fostering global cooperation on climate change mitigation initiatives is vital. The influence of climate change transcends borders, necessitating a united front to reduce greenhouse gas emissions and invest in sustainable practices. Additionally, funding mechanisms that support the development of healthcare capacity in high-risk regions can alleviate some of the burdens posed by extreme heat events.
In summary, the relationship between heatwaves and healthcare is increasingly critical as the world grapples with the ramifications of climate change. The escalating frequency and intensity of heatwaves pose direct threats to public health and challenge the efficacy of healthcare systems globally. Understanding these dynamics and approaching them through the lens of sustainability and equity can help mitigate the burdens imposed by this environmental phenomenon. Collaboration across sectors, implementation of robust public health policies, and proactive community engagement are paramount to safeguarding health in an era of climate instability.