Climate change, often depicted as an abstract phenomenon, is, in essence, a slow-burning crisis that models the gradual nibbling away of a foundational ecosystem; an insidious predator stalking its prey. As we navigate through the complexities of this global challenge, the intricate web of interconnections between our environment and public health becomes starkly apparent. While we may focus on direct threats like pollution and extreme weather events, there is a myriad of indirect, yet equally crucial, health ramifications lurking beneath the surface.
At the forefront of the climate-health nexus is the increasing prevalence of respiratory illnesses. As the climate warms, the concentration of air pollutants—such as particulate matter and ground-level ozone—tends to rise. This sweeping transformation morphs our atmosphere into a veritable cauldron of harmful substances, disproportionately affecting vulnerable populations: children, the elderly, and those with pre-existing health conditions. Asthma rates have soared, and hospitals have become synonymous with overcrowded emergency rooms, where respiratory ailments have become the new epidemic.
Furthermore, vector-borne diseases, once confined to specific geographical locales, are beginning to infiltrate new territories like uninvited guests at a party. The intricacies of climate change facilitate the transmission of diseases such as malaria, dengue fever, and Zika virus. Warmer temperatures and altered rainfall patterns create ideal breeding grounds for the mosquitoes that carry these pathogens, effectively rewriting the map of where these diseases can thrive. The notion of a “healthcare refugee” is emerging—a grim testament to those displaced not by conflict, but by encroaching climates reshaping their environments.
As we delve deeper, it is imperative to unpack the emotional and psychological toll of climate change. The collective anxiety stemming from climate-induced disasters is palpable. Individuals, full of dread and uncertainty about the future, grapple with what is often termed “eco-anxiety.” Mental health issues are exacerbated following extreme weather events, further convoluting the public health landscape. The psychological weariness experienced by those in affected communities parallels the physical toll borne by the toll of climate change—both are debilitating and require a concerted response.
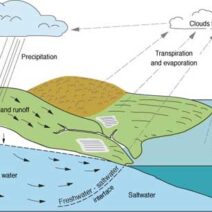
Moreover, access to clean water is becoming a harrowing issue as our climate continues to evolve. Changing precipitation patterns and prolonged droughts are jeopardizing water supplies, particularly in already marginalized areas. As rivers run dry and aquifers deplete, the consequences are manifold: the rise of waterborne diseases, food scarcity, and social disintegration. Each drop of clean water is akin to liquid gold, coveted and contested, further stoking the flames of inequality.
Agricultural systems are also not immune from the grip of climate change. As the viability of arable land fluctuates due to soil degradation, invasive species, and shifting weather patterns, food security becomes an urgent public health issue. The delicate balance of our food systems resembles a house of cards; once disrupted, it threatens to topple, leaving hunger in its wake. Malnutrition rates are poised to surge as staple crops fail to yield, pushing vulnerable populations deeper into the abyss of food insecurity.
In the grand tapestry of global health, socioeconomic factors play an indispensable role. Communities that are economically disadvantaged often bear the brunt of climate change’s health impacts. The thread of inequality weaves through every facet of public health, exposing deep-rooted disparities. Access to healthcare resources, public health infrastructure, and education profoundly influences resilience to climate impacts. Addressing these inequities is crucial for fostering a healthier society; otherwise, the chasm between the privileged and the dispossessed will widen, creating a recipe for civil unrest and societal discord.
To combat this multifaceted crisis, a holistic and multi-pronged approach is essential. Public health professionals must become adept storytellers, crafting narratives that intertwine climate change and health in compelling ways. Education is paramount; communities must understand the intricate connections between their health and the environment to advocate for systemic changes. Furthermore, policymakers must prioritize climate action as an essential component of public health strategies, recognizing the interdependence of the two realms.
Engagement at grassroots levels can catalyze transformative actions. Initiatives that promote local resilience, sustainable practices, and carbon reduction strategies can address both environmental and health disparities. Urban planning that integrates green spaces and efficient transport can diminish air pollution, benefitting respiratory health. Additionally, reforestation projects can enhance mental well-being by creating spaces conducive to recreation and solace, allowing communities to rejuvenate amidst adversity.
In conclusion, climate change represents a global health crisis that transcends the physical realm; it is a profound, systemic challenge intertwined with social justice, mental well-being, and economic stability. It interrogates our humanity, echoing through the chambers of public health as it raises critical questions about our future—how we nurture our planet, confront our interdependencies, and address the inequities that emerge in its wake. The urgency of addressing climate change cannot be overstated, as failing to do so will manifest in irreversible consequences for health systems worldwide. Addressing this crisis is not merely an environmental imperative, but a moral obligation as stewards of our planet and champions of public health.