As the planet warms due to human-induced climate change, a corollary phenomenon emerges in the form of increased disease outbreaks. This relationship is often obscured by the complexities of both environmental science and epidemiology, yet it is critical to delineate how global warming exacerbates the transmission and emergence of infectious diseases. By examining the interplay between climate dynamics and pathogen ecology, we illuminate the pathways through which rising temperatures facilitate an increase in virulent outbreaks.
The observable manifestation of climate change—rising temperatures, erratic weather patterns, and extreme climatic events—creates a perfect storm for the proliferation of infectious agents. Pathogens such as viruses, bacteria, and parasites are inherently sensitive to ecological conditions. For instance, temperature fluctuations can influence the development and survival rates of these pathogens, altering their replication cycles, infectivity, and ultimately, their geographical distribution.
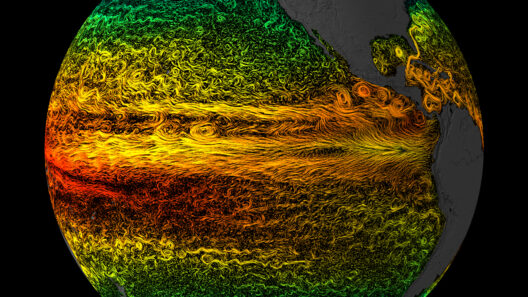
One of the fundamental mechanisms at play is the effect of temperature on vector-borne diseases. Vectors, such as mosquitoes and ticks, thrive in warmer conditions. The expansion of their habitats due to rising temperatures enables these vectors to invade new territories, thereby facilitating the transmission of diseases like malaria, dengue fever, and Lyme disease to previously unaffected regions. As climatic zones shift, so too do the ranges of these vectors, bringing pathogens into contact with new populations and amplifying the risk of outbreaks.
In addition to vectors, the persistence of pathogens in the environment is heavily influenced by climatic variables. For example, warmer temperatures can enhance the viability of bacteria in water sources, leading to heightened risks of waterborne diseases such as cholera. Flooding, another consequence of climate change, can exacerbate this issue by contaminating clean water supplies and creating conditions ripe for disease transmission. The interplay between rainfall patterns and pathogen dynamics is intricate, with excessive rainfall leading to stagnant water bodies that serve as breeding grounds for disease vectors.
The role of zoonotic diseases in this context cannot be overstated. Many emerging infectious diseases originate in wildlife populations before spilling over into human populations, a process termed “zoonotic spillover.” Climate change alters wildlife habitats and migration patterns, forcing animals to adapt in ways that bring them into closer contact with agricultural practices and human settlements. This interaction increases the likelihood of zoonotic disease transmission. Notable examples include the transmission of the Nipah virus and SARS-CoV-2, both of which have roots in wildlife and have led to significant public health crises.
Correlatively, climate-induced disruptions can lead to socio-economic vulnerabilities that further compound the risks associated with disease outbreaks. Communities experiencing climate stresses, such as food insecurity and displacement, may find their healthcare systems overwhelmed or ill-equipped to manage increased disease incidence. As resources become scarce and living conditions deteriorate, the potential for outbreaks escalates. The intersection of climate impacts and health equity is particularly salient here; marginalized populations often bear the brunt of such crises, highlighting the ethical dimensions of climate change and health.
Moreover, alterations in biodiversity due to climate change can have profound implications for disease dynamics. A decrease in biodiversity may reduce the natural checks on pathogen populations, fostering environments where diseases can thrive unchecked. Ecosystems with rich biodiversity often exhibit a phenomenon known as the “dilution effect,” in which a variety of species can disrupt transmission dynamics and mitigate the spread of pathogens. However, as habitats are altered or destroyed through human activities, this protective effect diminishes, leaving human populations more susceptible to outbreaks.
One cannot overlook the psychological and sociological dimensions of climate change and disease, either. The increasing frequency of pandemics generates a pervasive anxiety in societies globally. This anxiety is not unfounded; the impacts of climate change on health are expected to escalate as the planet continues to warm. Public consciousness is rising regarding the need for resilience strategies that address both environmental sustainability and public health. Interdisciplinary approaches that integrate environmental science, epidemiology, and social equity are essential for developing effective interventions.
Lastly, it is vital to underscore the imperative of action. Addressing the underlying causes of climate change is not merely an environmental concern but a profound public health mandate. Comprehensive strategies to mitigate greenhouse gas emissions, promote sustainable land use, and protect biodiversity are integral not only to combat climate change but also to stave off the impending risks associated with unfettered disease proliferation. Global cooperation is paramount; climate change knows no borders, and neither do the pathogens it empowers.
In conclusion, the interconnectedness of climate change and disease outbreaks emphasizes a critical need for integrated approaches to health and environmental policy. The phenomena we observe today serve as a clarion call, highlighting that the health of our planet is inextricably linked to the health of its inhabitants. As the impacts of climate change continue to unfurl, safeguarding human health will require an urgent and concerted effort to address environmental degradation, prompting a collective reevaluation of our relationship with the natural world.