Global warming presents a multitude of challenges that extend beyond the environmental realm, directly impacting human health, particularly for those with pre-existing medical conditions. As our planet’s temperature rises, the physiological responses elicited in our bodies become increasingly critical. This discourse navigates through the intricate connection between climate change and heart health, elucidating how rising temperatures can exacerbate cardiovascular issues and jeopardize the well-being of those affected.
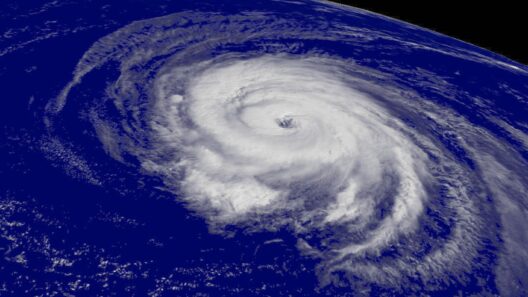
The primary concern surrounding global warming is not solely the increase in average temperatures but also the resultant extreme weather patterns that accompany it. Heatwaves, flooding, and severe storms have become more frequent, each posing unique threats to public health. These climatic phenomena can precipitate acute episodes of stress for individuals with complicated health histories—especially those with cardiovascular diseases. Research indicates that elevated temperatures can intensify heart strain, leading to a cascade of risks such as heart attacks and strokes.
Individuals with pre-existing conditions like coronary artery disease, hypertension, and heart failure are particularly vulnerable during sweltering conditions. The heart must pump harder in an attempt to maintain normal body temperatures. Such physiological exertion can lead to arrhythmias or heart failure. Moreover, exposure to high heat without adequate hydration can lead to dehydration, which in turn increases blood viscosity, further straining the heart’s capacity to function optimally.
Additionally, prolonged heat exposure can have dire psychological effects, worsening chronic conditions that may already affect heart health. Anxiety and depression often escalate during heatwaves. These emotional factors contribute to physical imbalances in the body, which can lead to the exacerbation of cardiovascular issues. The interplay between psychological stressors and physical heart health poses a vicious cycle that compounds risks for already vulnerable individuals.
Tackling heart health amidst the backdrop of climate change requires understanding the multifaceted nature of the crisis. Urban areas experience what is known as the “urban heat island” effect, where concrete, asphalt, and minimal greenery contribute to higher localized temperatures. People living in these densely populated environments are often more affected than their rural counterparts, primarily due to exacerbated pollution levels and limited access to green spaces. Consequently, urban populations generally face heightened risks of cardiovascular complications, making it imperative to address urban planning in light of climate change considerations.
The elderly population represents another demographic group that experiences extraordinary exposure to the harmful effects of global warming. As age progresses, pre-existing heart conditions become more common, and resilience to heat diminishes. Furthermore, older individuals may have diminished physiological capacity to self-regulate their body temperatures, hastening the need for intervention during extreme heat events. Communities must leverage resources such as cooling centers to mitigate these risks, alongside broader systemic changes to combat climate change.
Compounding these climate impacts are the air quality concerns associated with rising temperatures. Increased heat can lead to higher concentrations of ground-level ozone and other pollutants. These adverse air quality outcomes can aggravate respiratory and cardiovascular health conditions. For those with asthma or chronic obstructive pulmonary disease, the intersection of poor air quality and heat can be particularly lethal. Consequently, managing heart health must encompass a holistic approach that integrates strategies for improving overall environmental health.
Climate-induced migration also plays a crucial role in cardiovascular health. Individuals uprooted due to rising sea levels or extreme droughts often face the dual challenges of precarious lifestyles and deteriorating health systems. This displacement can exacerbate stress levels, leading to increased rates of heart disease among affected populations. Preventative measures must be considered in policy-making to protect these vulnerable communities, ensuring they have access to medical care and mental health support during transitions.
As the intersection of climate change and heart health becomes increasingly apparent, public health initiatives must prioritize education and outreach. Programs must empower individuals, especially those with pre-existing conditions, to recognize the symptoms and warning signs of heat-related distress. Health care systems should integrate climate resilience into patient education. Creating awareness regarding hydration, the importance of recognizing heat stress symptoms, and promoting regular health screenings can enhance proactive measures for heart health amidst the changing climate.
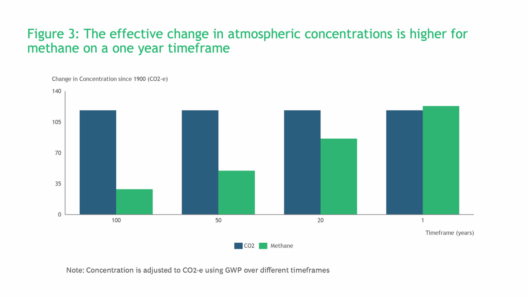
On a broader scale, systemic change is essential. Policymakers must enact legislation reflecting the urgent need to combat climate change, focusing on sustainable public health strategies. Initiatives to reduce greenhouse gas emissions, improve urban infrastructure, and enhance public transportation can significantly mitigate health risks associated with climate change. Such endeavors not only improve air quality but also foster healthier living environments, ultimately reducing cardiovascular risks in the process.
In conclusion, the nexus between global warming and cardiovascular health concerns is both complex and concerning. Heart health, particularly for individuals with pre-existing conditions, faces unprecedented challenges amidst our evolving climate. Proactive community engagement, along with concerted policy efforts, can mitigate these risks. The urgency to act in protecting our environment translates into safeguarding our health and, ultimately, preserving the well-being of our communities.